The Basics of Antimicrobial Resistance
- antimicrobial
- one health
- antimicrobial resistance
- bacteria
- antibiotics
- superbugs
- antibiotic
- super
- amr
- bugs
- When prescribed a course of antimicrobial, be sure to comply to the correct dosage AND duration as directed by your doctor.
- Never end a course of antimicrobials early without direct instruction of your doctor.
- Use diagnostic tests prior to treatment such as a culture and sensitivity to rule out causes of infection such as bacterial or fungal.
- Do not treat viral infections with antibiotics.
- Ask your doctor about symptom management when antimicrobials are not necessary.
- Practice good hygiene.
- Prevent infections through your hospital’s infection control program and client communication, not through use of antimicrobials.
- Utilize symptom management, especially when the disease is self-limiting, so the client feels they were listened to are being helped.
- Use diagnostics such as culture and sensitivity to identify the need for antimicrobials and which spectrum to use.
- Classify your hospital’s antimicrobials into groups of primary, secondary, tertiary, and restricted.
- Communicate with hospital staff on clinical situations where empirical treatment is appropriate.
- Utilize proper PPE (personal protective equipment) and practice good hygiene.
-
Maintain detailed records.
-
Proper case follow-up
Antimicrobials are designed to treat infections caused by microorganisms such as bacteria, protozoa, and fungi. These drugs target parts of the infective microorganism such as the cell itself, or its mechanisms of survival like metabolism and synthesis. Unfortunately, bacteria are capable of developing resistance to antimicrobials, whereby specific drugs are no longer effective at treating infections. Overuse and misuse led to the immense problem today of antimicrobial resistance (AMR) in both human and veterinary medicine.
AMR arises from imprudent use of antimicrobials. Examples of inappropriate use include using antimicrobials in situations that are medically unnecessary, owner noncompliance, using the incorrect drug, dose or duration, and use as a preventative measure. There is little information readily available about antimicrobial use practices and AMR in the veterinary and dog breeding communities. Furthermore, national and international efforts in this area are disjointed with limited resources for these communities to guide optimum behaviors. This project has great significance in that it aims to bridge existing knowledge gaps across multiple interest groups and countries and help reshape behaviors of those inappropriately using antimicrobials.
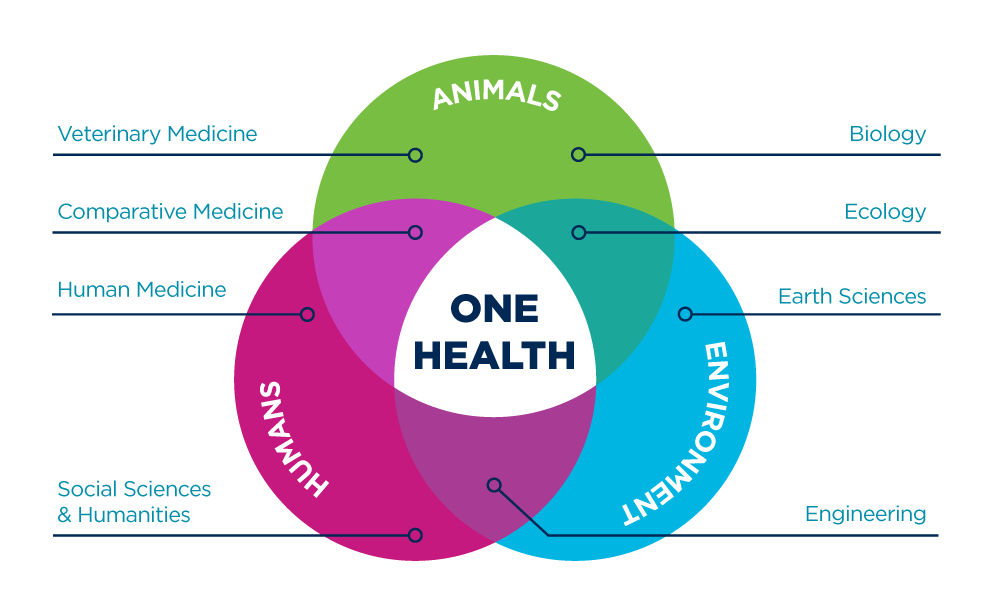
AMR is a public health pandemic of which multiple stakeholders are contributing. The breadth of AMR expands far past inappropriate overuse of z-packs at the local convenient store doctor. Other contributors you may not think of are veterinarians, breeders, patients, farmers, and many more. Resistant strains of microbes are lurking in so many different places, from the food industry to when you take your own pet to the veterinarian. This is why having a ‘One Health’ perspective is absolutely essential to tackling this difficult issue.
The concept of 'One Health' is captured well in this venn-diagram from UC Davis.
Essentially, we need to put our pride aside, and stop debating who are the "real doctors." We need to realize we all have something unique to bring to the table, and if we work together instead of in opposition, we are much more likely tackle this issue.
Recommendations for the general public:
Recommendations for veterinarians:
Downloadable guidelines and pamphlet from the ISCAID and the ODH for your clinic:
AAHA and AAFP Guidelines for Prudent Antimicrobial Use in Companion Animal.pdf
This article is part of the IPFD Student Project 2017 by Ariel Minardi.
For an overview of her project and links to other material on Antimicrobial Resistance (AMR) and Prudent Use of Antibiotics see:
IPFD Student Project 'B.A.R.K. | Bacterial Antimicrobial Resistance Knowledge' - Overview
References:
A. M. Sefton “Mechanisms of Antimicrobial Resistance” Drugs Vol. 62, Iss. 4, 2002.
Center for Disease Control "Healthcare Associated Infections: What Patient's Can Do" U.S. Department of Health & Human Services, 2017
H. Harbottle, S. Thakur, S. Zhao, and D. G. White “Genetics of Antimicrobial Resistance” Animal Biotechnology Vol. 17, Iss. 2, 2006.
"Unique One Health Collaborations." UC Davis, 2017.
The Ohio State University Veterinary Public Health Program "Prudent Antimicrobial Use in Companion Animals to Prevent the Emergence & Spread of Multidrug-Resistant (MDR) Pathogens" Ohio Department of Health, 2017.
Edited by Ariel Minardi
Report Entry
 Donate
Donate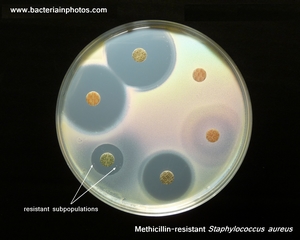

Recommended Comments
There are no comments to display.
Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.
Note: Your post will require moderator approval before it will be visible.